COVID-19 Library
The COVID-19 pandemic represents an unprecedented global public health crisis. Oral health professionals, dental associations and regulatory bodies are facing diverse challenges to continue providing dental care and promoting the oral health of the population, while at the same time protecting patients and practitioners from the health threat posed by SARS-CoV-2.
This library contains guidance for oral health professionals and other resources relating to the COVID-19 pandemic issued by national and international bodies.
Mental Health of Dental Professionals
Several surveys have been carried out to assess the mental health of dental professionals. According to a survey carried out by the Dental Defense Union in the UK, 68% of dental professionals believe their anxiety and stress levels increased since the pandemic started.
The American Dental Association (ADA), together with a non-profit movement named Hope for the Day, have put together resources to help professionals with their mental health. In these resources, they have also provided contact numbers across Europe, UK and the US to help people in need regarding their mental wellbeing and preventing suicide.
The association between periodontal health, the use of mouthwash, oral hygiene and SARS-CoV-2
Periodontitis has already been associated with many non-communicable diseases (NCDs), such as diabetes, hypertension and cardiovascular diseases. A recent study suggested that periodontitis may be associated with an increased risk of COVID-19 complications. Patients presenting periodontitis were 8.8 times more likely to have complications when tested positive for COVID-19.
The study highlights the importance of oral hygiene and periodontal health for preventing complications from COVID-19, as they suggest the mouth might act as a reservoir of SARS-CoV-2. A literature review emphasized that SARS-CoV-2 is found in the gingival fluid of COVID-19 patients, and that poor oral hygiene may increase the viral load in themouth and the risk of mouth-lung exchanges in terms of virus and bacteria.
A pilot trial investigated if the use of mouthwashes could reduce the viral load of SARS-CoV-2 in patients’ mouth. It concluded that the use of different types of mouthwashes help to temporarily reduce the viral load of SARS-CoV-2 for at least 30 minutes in the saliva of COVID-19 patients. The results may suggest a potential for mouthwashes to be used as a mitigating factor in dental practices, pending further conclusive research, along with the use of masks, handwashing, social distancing and decontamination of surfaces.
A few questions regarding periodontal health and COVID-19 have also been answered by one of the experts from FDI’s Global Periodontal Health Project, Prof. David Herrera.
Sustainability in Dentistry & COVID-19: a challenge.
Although health care professionals are aware that the care provided to patients needs to be delivered in a sustainable manner, the COVID-19 pandemic posed a major challenge to worldwide sustainability.
Face mask use is recommended widely to mitigate the spread of coronavirus disease, resulting in a global use of 129 billion face masks per month, the majority being disposable. They are generally made from plastic microfibers (polyester, polypropylene and polystyrene) and incorrect disposal is a threat for the environment. As with any other type of plastic, masks are likely to accumulate and release harmful substances and their elastic straps can be dangerous for wildlife, tangling them around it.
There is urgent need for the development of biodegradable masks that are safe to be used in different settings and accessible to the wider public. While these are not available, a few other tips can mitigate the environmental impact of mask use.
The FDI Sustainability in Dentistry project aims to raise awareness of the importance of sustainable actions in dentistry and in the dental community. Together with our Task Team, we have provided resources that can help dental practices and communities make dentistry more sustainable. One of these is an infographic that can also be shared with patients in different languages.
Tracking SARS-CoV-2 Variants & Vaccination
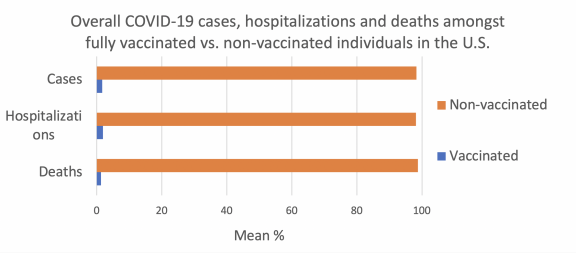
According to the Centers of Diseases Control and Prevention (CDC), the Delta (B1.617.2) variant was responsible for 99.1% of cases as of the end of August 2021 in the U.S., following the same trend (99.3%) of other 17 countries in the European Union and European Economic Area (EU/EEA), according to the European Centre for Disease Prevention and Control (ECDC).
The trends related to the uptake of vaccines are also very similar between these two regions, with 74.8% of adults (>18 years old) with at least one dose of the vaccine in the U.S. and 75.9% in the EU/EEA.
Although the vaccines provide a high protection against the SARS-CoV-2, fully vaccinated individuals can still become infected and transmit the virus to the others, asymptomatic or not. The Delta variant is more transmissible compared to previous variants; however, it can be detected earlier after exposure.
25 February 2021
COVID-19 continues to have a severe impact on global health, society and economies. Vaccines are essential in fighting the pandemic as they can protect people from getting ill and ease reliance on non-pharmaceutical public health measures, such as service closures and stay-at-home orders[i]. Several COVID-19 vaccines have been approved for use, having proven safe and effective in large-scale clinical trials. Over 200 other vaccine candidates are in various stages of development[ii]. As of late January 2021, nearly 100 million COVID-19 vaccine doses have been administered in over 50 countries, mostly to vulnerable populations such as the elderly and at-risk groups like healthcare workers[iii].
As countries begin implementing vaccination programmes, there is a need to highlight several considerations relating to dental services and the oral health workforce. Oral health is a fundamental component of overall health and wellbeing[iv],[v] and oral health care is an essential public service. Vaccination of dentists, their team members and other oral health professionals is important to contribute to continued access to care. Dentists are also highly trained professionals that have regular interactions with people about their health, and are therefore well positioned to support national vaccination programmes.
Considering these points, FDI Council asserts the following key principles related to dentistry and COVID-19 vaccination:
- Dentists, other oral health professionals and support staff are front-line providers of an essential health care service and should therefore be included in priority vaccination groups. They are in regular contact with each other and the patients who visit their healthcare facilities. If they contract COVID-19, it can result in practice or clinic closures. Including them in priority vaccination groups is therefore important for avoiding oral health workforce dropout and jeopardizing access to care.
- Equitable access to COVID-19 vaccinations is needed for the health of people globally, including vulnerable populations and healthcare workers. To this end, FDI Council fully supports initiatives to improve access to vaccines in underserved localities, such as the COVAX facility being co-led by GAVI, WHO and CEPI[vi].
- Efforts should be made to enable dentists to administer COVID-19 vaccines when possible within national legislation and regulations, and with minimal disruption to oral health care services. Several countries have already confirmed that dentists will be permitted to administer COVID-19 vaccinations, including in countries where dentists have not previously been permitted to give vaccines[vii].
- Dentists are well positioned to provide evidence-based information about vaccination and may receive questions from their patients about COVID-19 vaccines. Health authorities and National Dental Associations should ensure dentists, their team members, other oral health providers and dental students have access to accurate, up to date information on the vaccines available in their country or locality and the specificities of the vaccination programme in place.
- Given the expected large number of vaccine approvals and high population uptake in the near future, there may be a higher number of suspected adverse drug reactions than in normal times. Dentists can play an important role in pharmacovigilance programmes. Health authorities and National Dental Associations should ensure dentists are well informed of national pharmacovigilance systems and methods for reporting suspected adverse events.
FDI Council expresses its sincere thanks to all oral health professionals, National Dental Associations and other members of the global oral health community for their dedication in responding to the ongoing crisis.
Please visit the FDI COVID-19 RESOURCE LIBRARY for access to practical resources and more information on the outbreak.
Downloads :
FDI Council Statement on COVID-19 Vaccination
[i] World Health Organization. Vaccines and Immunization: What is Vaccination? Available from: https://www.who.int/news-room/q-a-detail/vaccines-and-immunization-what-is-vaccination [Accessed 2 February 2021].
[ii] GAVI: The Vaccine Alliance. The COVID-19 Vaccine Race – Weekly update, 27 Jan 2021. Available from: https://www.gavi.org/vaccineswork/covid-19-vaccine-race [Accessed 2 February 2021].
[iii] Ritchie H, Ortiz-Ospina E, Beltekian D, et al. Coronavirus (COVID-19) Vaccinations. Available from: https://ourworldindata.org/covid-vaccinations [Accessed 2 February 2021].
[iv] Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Int Dent J 2016 66: 322-324.
[v] World Health Organization. Oral Health: Achieving better oral health as part of the universal health coverage and noncommunicable disease agendas towards 2030. Report by the Director General. Executive Board 148th Session 2020. Available from: https://apps.who.int/gb/ebwha/pdf_files/EB148/B148_8-en.pdf [Accessed 5 February 2021].
[vi] GAVI: The Vaccine Alliance. COVAX Facility. Available from: https://www.gavi.org/covax-facility#what [Accessed 2 Ferbruary 2021].
[vii] In a survey of 57 National Dental Associations conducted by FDI in December 2020 and January 2021, 17% reported that their country has already confirmed that dentists are or will be permitted to administer COVID-19 vaccinations.
After its emergence in December 2019, COVID-19 has grown to pandemic proportions with over 5.7 million cases and 350,000 deaths confirmed in over 200 countries as of the beginning of June 2020. COVID-19 is not only negatively impacting people’s health, but also economies, education, productivity and the overall strength of health systems. The lack of effective treatment or vaccine means that infection control through non-pharmaceutical public health measures currently appear to be the only means to combat the pandemic1.
The outbreak is causing significant disruption to dental practice worldwide. Oral health professionals, dental associations and regulatory bodies are facing diverse challenges to continue providing dental care and promoting the oral health of the population, while at the same time protecting patients and practitioners from the health threat posed by SARS-CoV-2. Dental care is unique in that many procedures are performed with an average of around 35cm space between the patient’s mouth and the practitioner’s face2. Some dental procedures generate a large number of droplets and aerosols, therefore special attention and consideration are required in developing care guidelines and regulations during the pandemic3. The continuing operation and long-term survival of many dental practices is also threatened by the economic and social challenges arising due to care restrictions, practice closures and shortages of personal protective equipment (PPE), as well as the need of investing in new types of PPE and technology4.
As this is a new biological threat, there is a lack of knowledge and tools with which it can be fought. Evidence about how SARS-CoV-2 is spread and infects people is currently lacking and many of the public health decisions and recommendations in place are based on what is known about similar viruses. There is therefore a need to continuously review and update recommendations. Health professionals may need to update and change behaviours in-line with evidence as it evolves.
Guidelines and regulations to manage these challenges are being developed by appropriate national bodies, and oral health professionals are rapidly reviewing and implementing new guidance and requirements.
In view of this, FDI Council recommends some key principles for dental practice and oral health promotion during the current pandemic:
- Oral health is a fundamental component of overall health and well-being5, and oral healthcare is an essential public service that must be made as broadly accessible as possible. Authorities should ensure regulations do not unnecessarily impede access to oral healthcare and put measures in place to improve access where feasible, including tele-dentistry services, emergency clinics and oral health promotion initiatives.
- Oral health professionals and oral healthcare should be included in all discussions and decisions related to the regulation and guidance of healthcare delivery and health professionals during the pandemic.
- Where possible and relevant, authorities should provide appropriate financial and administrative support to dentists as business owners and liberal professionals, and implement appropriate fiscal measures, to reduce the financial burden on dental practices and ensure the continuation of adequate care during and after the pandemic.
- All regulations and guidance for oral health professionals and oral healthcare should take into account the current public health situation and needs of the country, and not only the individual infection risk of practitioners and patients.
- Oral health professionals must strictly follow all national guidelines and regulations in place, including those relating to personal protective equipment (PPE), treatment procedures and patient intake procedures.
- Authorities should ensure easy access to PPE at reasonable costs.
- Oral health professionals have a responsibility to assure emergency care whenever possible and as permitted by national regulations.
- Oral health professionals should take every opportunity to communicate and reinforce oral disease prevention messages to help reduce treatment need, avoidable dental visits and healthcare costs.
- Dentists/practice owners have a responsibility to protect the health and well-being of their staff and patients.
- Further research into SARS-CoV-2 and its transmission, including specific considerations for dental practice, is essential to allow appropriate guidance to be made.
FDI Council expresses its sincere thanks to the global oral health community for their dedication in responding to the ongoing crisis.
1 World Health Organization. Surveillance strategies for COVID-19 human infection: Interim Guidance 10 May 2020. Geneva: World Health Organization;2020. Available from: https://www.who.int/publications-detail/surveillance-strategies-for-covid-19-human-infection [Accessed 2 June 2020].
2 Wajngarten D, Garcia PP. Effect of magnification devices on dental students’ visual acuity. PloS one. 2019;14(3).
3 Thamboo A, Lea J, Sommer DD, et al. Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology – head and neck surgery during the COVID- 19 pandemic. J Otolaryngol Head Neck Surg 2020;49(1):28.
4 European Centre for Disease Prevention and Control. Safe use of personal protective equipment in the treatment of infectious diseases of high consequence. Stockholm: ECDC;2014; Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J Dent Res. 2020; Apr 17.
5 Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new defintion for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Int Dent J 2016 66: 322-324
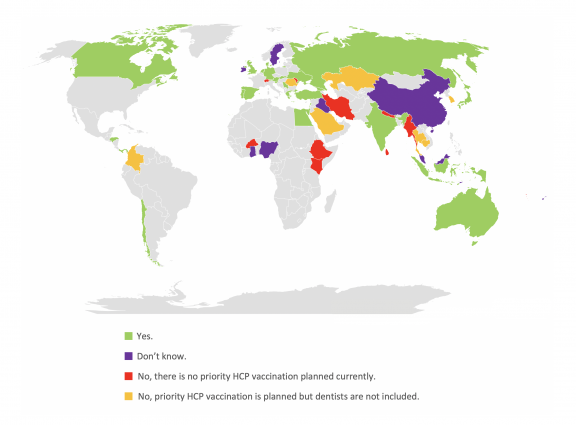
Will oral health professionals be included in a priority vaccination programme for healthcare professionals (HCPs) in your country?
The COVID-19 Task Team oversees the development and implementation of FDI’s COVID-19 strategy, which is centred around three goals: support members in mitigating the risk from COVID-19 to health and daily practice; ensure continued access to care and promote prevention strategies for oral health; and to represent the profession when political and economic priorities are reshaped.
| Title | Source | Resources |
|---|---|---|
| Recomendaciones para la atención exclusiva de emergencias y urgencias odontológicas durante la pandemia por COVID-19 | Colegio de Cirujanos Dentistas de Costa Rica |
|
| Recomendaciones para la guía de apertura de los servicios odontológicos en la República Dominicana debido a la pandemia COVID-19 | Colegio Dominicano de Odontólogos, Asociación de Clínicas Dentales Dominicanas, Servicio Nacional de Salud |
|
| Recomendaciones para la práctica odontológica | Gobierno de México |
|
| Recomendaciones para la práctica odontológica ante COVID-19 | Subsecretaría de Prevención y Promoción de la Salud, Centro Nacional de Programas Preventivos y Control de Enfermedades, Dirección General |
|
| Recomendaciones para prevenir el contagio por COVID-19 en el consultorio dental | Secretaría de Salud, Comisión Nacional de Arbitraje Médico |
|
| Recomendações para situações de urgência e inadiáveis | Ordem dos Médicos Dentistas |
|
| Recommandations COVID-19 | Chambre Syndicale Dentaire (CSD) |
|
| Recommandations de prise en charge des soins bucco-dentaires en période post-confinement | L'Ordre National des Médecins Dentistes du Maroc, La Fédération Nationale des Syndicats des Médecins Dentistes du Secteur Libéral |
|
| Recommendations du conseil national de l'Ordre des Chirurgiens Dentistes du Burkina Faso | Association des Chirurgiens-Dentistes du Burkina Faso (ACDB), Ministère de la Santé du Burkina Faso |
|
| Recommendations for the re-opening of dental services: a rapid review of international sources | COVID-19 Dental Services Evidence Review (CoDER) Working Group |






